Chronic Pain
This webpage has been put together by our clinical team that provide information, management and support for patients suffering with chronic pain issues.
Specifically, below is information on:
- the different types of chronic pain
- the different types of prescribed treatment available in general practice
- frequently asked questions
- Information and links to community and hospital clinics for chronic pain.
- Online support, videos links, and further links to explore further the different types of chronic pain such as headaches , fibromyalgia, IBS & arthritis.
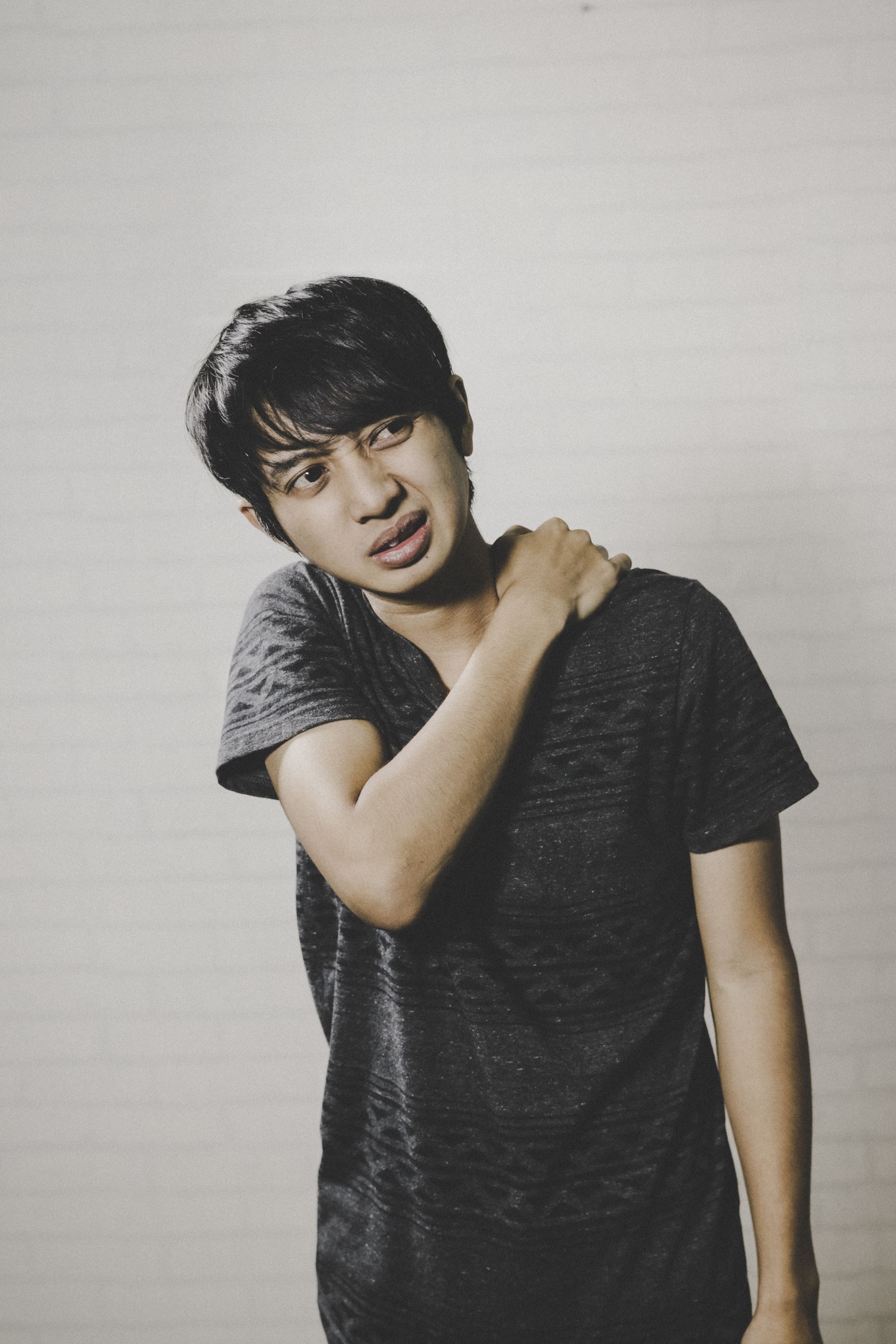
What is Chronic Pain?
Chronic pain is when pain lasts for more than 3 months. It can also be referred to as long-term pain or persistent pain. It is one of the biggest causes of disability in the UK and affects 1 in 5 people in Scotland.
It can significantly affect individuals especially when uncontrolled or poorly managed. This often leads to increased suffering, impact on daily function and worsening mental health.
Chronic pain can be caused directly by an underlying medical condition such as cancer or common condition like arthritis (chronic secondary pain) . However, many causes of chronic pain have no underlying specific origin and are what we describe as functional pain (chronic primary pain). In this situation, it is the function of the nervous system itself that is not working properly, often interrupting how a part of the body works and how the signals of pain are interpreted by the brain.
Both type of pain described above are very real for the person experiencing it but how they are managed can differ depending on the symptoms and underlying diagnosis.

Complications of Chronic Pain
Not only does chronic pain have a negative impact on physical health and daily activities, but it can also lead to:
- Depression and anxiety: it is estimated that around 48% of people with chronic pain also suffer from depression. If you believe you may be suffering from anxiety or depression, please visit our mental health page and book an appointment with your GP
- Poor sleep
- Increased risk of medication side effects as well as medication misuse and accidental overdoses
- An overall reduced quality of life daily living, family, social relationships, and employment can all be negatively affected
Types of Chronic Pain
Chronic Primary Pain
Chronic primary pain (functional pain)– below are some of the most common causes. Please click on list below for more information:
Chronic Secondary Pain
Chronic secondary pain – there are different types of chronic secondary pain:
- Arthritis causing joint pain.
- Nerve pain, also known as neuropathic pain. It is often described as a shooting pain, like an electric shock. This is caused by conditions that affect nerves, such as:
- Diabetic neuropathy, which is the most common cause of peripheral neuropathy in the UK
- Trigeminal neuralgia
- Shingles, also known as postherpetic neuralgia
- Multiple sclerosis
- Cancer pain is usually caused by the tumour pressing on bones, nerves, or other organs within the body. It can also be caused by the treatment you are receiving.
- post surgical / post-traumatic pain (fractures/ severe sprains)
- chronic abdominal pain from inflammatory bowel disease.
Medications Used To Treat Chronic Pain
Frequently Asked Questions
I’m still in pain despite starting medication - is that normal?
We usually start chronic pain medication on the lowest possible dose. Therefore, it can be common to experience some pain once you first start taking these medications. Please speak to your GP as soon as possible if you are still experiencing pain – you may need a medication review, or referral to a specialist team.
Will I get addicted to pain medications?
It is possible to become addicted to pain medications if they are taken for a long time. If this is something that you are concerned about, please speak to your doctor for a medication review.
What Happens if I Overdose on my Medications?
If you are worried that you have taken an overdose, please call 999 immediately. Signs of an opiate overdose include:
- Small pupils.
- Shallow or slow breathing.
- Drowsiness.
To aviod overdose, please only take the medications as prescribed and avoid taking them with alcohol or other recreational drugs.
What happens if I stop taking my pain medications?
If you stop taking your medications suddenly, you may feel unwell and experience what are called withdrawal symptoms. These can include stomach cramps, sweating and diarrhoea. Contact your GP or phone 111 if you experience any of these symptoms. Please do not stop taking the medications or changing your dose without speaking to your doctor first.
Can I drive if I’m taking pain medications?
There is a new law making it an offence to drive with levels of certain medicines in your body, including strong opioids. The law aims to target dangerous drivers after illegal use of medicines/drugs. So don’t worry– if you are taking one for medical reasons, you are still allowed to drive if you have taken it according to GP's instructions and your driving ability is not affected.
However, do not drive:
- If you feel drowsy;
- After taking other drugs that cause daytime drowsiness;
- After drinking alcohol;
- For at least 3 hours after taking a fast-acting/breakthrough strong opioid;
- For at least 5 days after starting or increasing the dose of a strong opioid.
Is there anything else I can do to help my pain?
It's important to continue with your normal activities as much as possible.
Exercising is important as lack of activity can worsen chronic pain. Good exercises include walking, swimming, cycling, and yoga. We also have a walking group every Thursday from 1-2pm, which you can read more about here.
Staying at work helps give you a sense of normality, and keeps you active, which is better for your mental health.
Physical therapy can help to relieve pain and make daily activities easier. Please speak to your GP if you would be interested.
Other ways to improve your lifestyle are a healthy diet, reducing smoking and alcohol. If you would like support for any of these, please book an appointment.
What Are The Signs of Overdose?
The signs of overdose are very different to the signs of a severe allergic reaction (also known as anaphylaxis). Call 999 or go to A&E now if you are experiencing any of the following:
- A new skin rash.
- Tightness in the chest and/or throat.
- Trouble breathing or talking.
- Swelling in your mouth, face, lips, tongue or throat.
Is There Any Mental Health Support Available for People with Chronic Pain?
Of course. On our Mental Health page, there are many mental health resources you can find. However please speak to your GP if this is something you would like to discuss further.
Do I Have To Tell DVLA?
You are not required by law to tell the DVLA if you are taking strong opioids, however insurance companies do advise this. You must inform your insurance company of any serious illnesses, otherwise you may not be covered.
For more information, visit the DVLA website or call their medical advisory helpline on 0300 890 6806.
Community Support

Exercise therapy
Exercise therapy is widely known to have benefits for long term chronic pain . Click here to find more about fit for Health scheme with Edinburgh Leisure.
NHS Lothian Chronic Pain Service
Is a multi-disciplinary specialist service comprising of a team of doctors, nurses, psychologists and physiotherapists. The teams operate pain clinics in several sites in Edinburgh.
The aim:
- To reduce chronic pain in sufferers as much as possible
- Helping people to learn to live with their pain and improve their quality of life as much as possible
Please note referral to the PMP and pain clinic service requires: patients to be over 16 years of age, had chronic pain for over 6 months, and pain that is significant in severity and disability.

The team offer 3 types of service:
- Specialist Pain Clinics - run at several different sites around the city, which focuses on optimisation of treatments for chronic pain
- Pain Management Programme (PMP)- run at the Astley Ainslie Hospital in South of Edinburgh is aimed at helping living with pain better.
- Online Cognitive behavioural Therapy (CBT)- provide online programme to help anxiety/depression related to chronic pain
Access to the first two services requires an initial assessment and referral by our clinical team here at Bangholm Medical Centre. You can access the online CBT through completing the online form below.
Pain Management Programme (PMP)
The Pain Management Programme is a specialist service that has been designed to help reduce the effect pain is having on an individual’s quality of life through self-management strategies.
The team comprises of experienced physiotherapist and psychologists that use a rehabilitative & psychological approach to pain self-management.
The course consists of both individual and group-based programmes.
Tel: 0131 537 9128
Specialist Pain Clinics
Specialist Pain Clinics are held at:
Leith Community Treatment Centre, Western General hospital and The Royal infirmary Hospital.
This service is usually a consideration when our clinical team have exhausted all possibilities through normal GP and community teams.
They are lead by chronic pain consultants who focus on:
- Assessment and conideration of further specialist investigations.
- Medication review and drug management.
- Injection therapy and complementary therapy.
Please note this service is not appropriate for patients with predominantly severe mental health issues or associated drug or alcohol dependency.
CBT for chronic pain- online programme
This online programme is designed for people with mild to moderate symptoms of depression and anxiety who are living with chronic pain.
The programme consists of weekly online sessions with support from the NHS psychology team
Video and Webinar Session on Chronic Pain
Tame the Beast
Is a great website that provide information about :
- why we feel pain and the science behind it
- the new approaches to tackling pain
- links to useful online resources, courses and videos
- real life stories

The NHS Inform website includes advice on common causes; when and how to take painkillers, when to see a doctor and helpful exercises (with video guides) to relieve pain. There is also a handy mobile app which contains exercises and has the option to set reminders. The Musculoskeletal Helpline is a free telephone advice service for people experiencing muscle or joint problems. Phone advisors can refer you to a physiotherapist or podiatrist if you need it.
- You can also call them: 0800 917 9390
- Or download their app here.

Action on Pain
Is a charity run by volunteers who are themselves affected from chronic pain in some way. the website provides helpful advice ,support and raising awareness of sufferers living with chronic pain. It also has good summaries of alternative therapies and useful techniques on managing chronic pain
Tel number: 0345 6031593
email address: painline@action-on-pain.co.uk
Links to specific types of chronic pain
Page created: 04 September 2020